The prevalence of autoimmune disease has increased exponentially over the last 20-30 years. It is reported that roughly 700 million people around the world are living with some sort of autoimmune condition.
“There’s no sign of this trend slowing down; on the contrary, the prevalence of autoimmune diseases like type 1 diabetes, inflammatory bowel disease, and multiple sclerosis is increasing at an alarming pace. From 2001–2009 alone, the incidence of type 1 diabetes increased by 23 percent!”
To add concern to the growing number of individuals living with the condition, it appears that conventional treatment has little to offer in reducing the severity and discomfort that accompanies autoimmune disease.
What is Autoimmune Disease?
The human body is designed with a specialized immune system composed of a complex network of special cells and organs. These cells and organs are designed to defend the body from germs and other foreign invaders.
At the core of your immune system is the ability to differentiate between “self” and “nonself”, or what is you versus what is foreign matter. Autoimmune disorders, or disease, occurs when the body’s immune system begins to attack and destroy healthy body tissue by mistake.
“Autoimmune diseases are born when your body is working hard to defend itself against something potentially dangerous, such as an allergen, a toxin, an infection, or even a food, and it fails to differentiate between the intruder and parts of your own body. Mistaking certain types of tissues for harmful substances, your body turns these antibodies against itself, wreaking havoc on your organs.”
Autoimmune disorders usually fall within one of two categories: systemic or local. Here is the difference:
- Systemic autoimmune diseases are linked to the production of non-specific tissue autoantibodies, leading to a spectrum of damage which can affect a wide range of tissues, organs, and cells of the body.
- Localized autoimmune diseases, on the other hand, lead to organ-specific conditions, affecting a single organ or tissue.
It is important to note, however, that the boundary between systematic and nonsystematic disorders can become a bit fuzzy as the disease runs its course. In other words, as the effect and scope of localized autoimmune disorders takes hold of the body, it is not uncommon for the damage to extend beyond the initially targeted areas.
Immune System 101
To better understand how your body has the ability to “attack itself”, leading to the development of an autoimmune disease, it helps to know the basics about immunology. Let’s briefly look at the various organs, the cells they produce, and the role these specialized cells play in protecting you from illness.
- Bone marrow –found within your bones, where immune cells are derived.
- Thymus – A flat, pinkish-gray gland, found in the upper chest in front of the heart. This is where your T-cells pass through and mature.
- Lymphatic system – A critical system for the elimination of toxic waste from your tissues. This system is made up of lymph fluid, lymphatic vessels, bone marrow, lymph nodes, spleen and tonsils.
- T-cells – These immune system cells function like “warriors” and mature in the thymus. Once mature t-cells enable each individual T-cell to recognize only one of millions of antigens, at which time they migrate into your lymphatic system and circulate in the blood.
- B-cells – These immune cells are produced in and by your bone marrow and are responsible for the secretion of antibodies.
You’ll notice the term “t-cells” used multiple times in the above list, and as you may have already gathered T-cells are of great importance. (#) These cells are taught to recognize invading cells, or non-self cells, from your own cells.
Remember, a normal functioning immune system only attacks substances and infections that are thought of as foreign invaders, such as cancer cells. When the immune system is “confused”, it begins to attack healthy cells found within the body.
Target Organs and Tissues
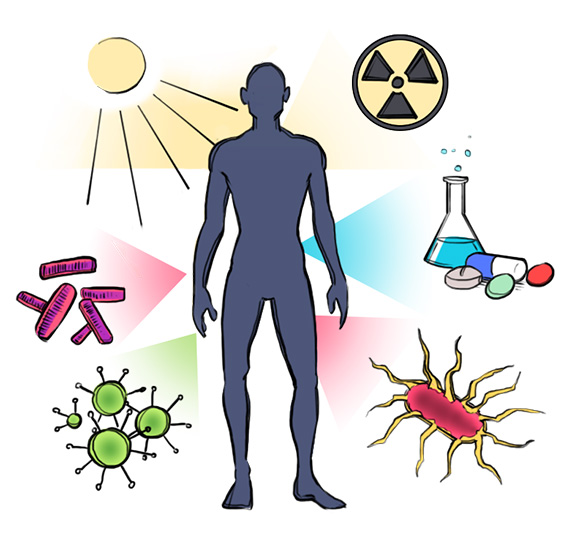
The triggers for autoimmune disorders are rather variable, and may be brought on by the following conditions:
- Environmental exposure to chemical solvents
- A drug response
- Contraction of a viral or bacterial infection
- Sunlight or radiation
Just as the triggers for an autoimmune reaction are varied, the debilitating effect vary as well depending on the target organs and tissues affected by disorders. (1) With more than 80 types of autoimmune disorders, some common tissue types and bodily sites that the immune system can begin to attack include:
- blood vessels
- connective tissue
- endocrine glands (i.e. thyroid or pancreas)
- joints
- muscles
- red blood cells, and
- skin
Keep in mind it is possible to have multiple tissues and organs attacked by the immune system, resulting in the diagnosis and presence of more than one autoimmune condition at the same time.
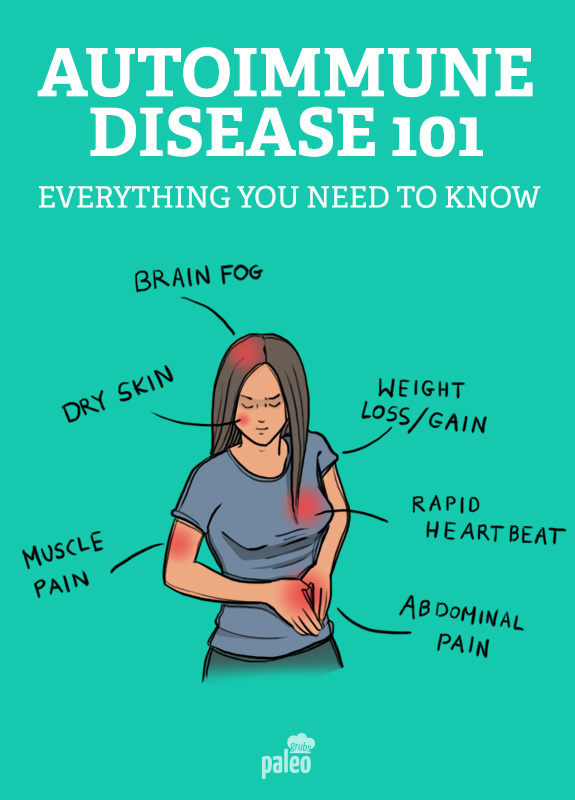
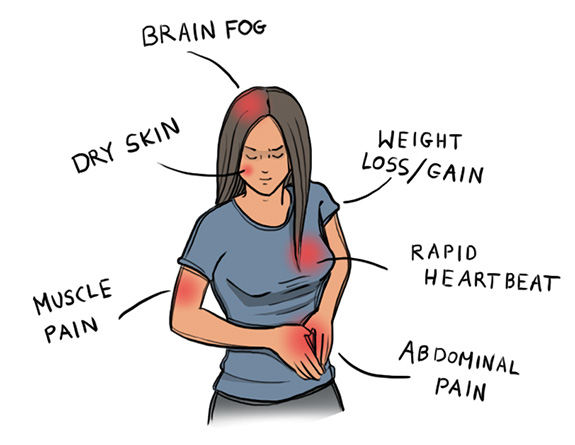
Signs and Symptoms of Autoimmune Disease
There is some amount of mystery and confusion behind certain autoimmune conditions, such as multiple sclerosis, rheumatoid arthritis and thyroiditis. (2) Part of what contributes to the unknown lies in the fact that the biological basis, and some of the most common symptoms that accompany such debilitating illnesses, may not be linked to one specific infection.
“Despite its prevalence, the level of basic autoimmune research funding is below 3% of the National Institutes of Health (NIH) total budget, which may explain why we understand so little about the roots of these diseases. Indeed, AARDA reports that the whole arena of autoimmune research is in its infancy…We do know there are factors at the root of autoimmune disease development, which include both genetic and environmental components.”
While the biological or genetic and environmental factors contributing to the development of an autoimmune disorder may not be well understood, there are some well documented signs and symptoms.
Experiencing any of the symptoms listed below may indicate the presence of an autoimmune disease; however, experiencing more than one of these symptoms could increase the likelihood of an autoimmune disorder:
- Joint pain or muscle pain, accompanied by weakness or tremors
- Unintentional weight loss or weight gain
- Insomnia
- Intolerance to heat or cold
- Rapid heartbeat
- Recurrent rashes or hives or sun-sensitivity
- Brain fog, difficulty concentrating or focusing
- Abdominal pain, bloody stools, diarrhea
- White patches or ulcers in and around your mouth
- Dry eyes, mouth, or skin
- Numbness or tingling in hands or feet
- Multiple miscarriages or blood clots
Gender Differences
It is estimated that up to 1/3 of the risk factors for developing an autoimmune stem from heredity and genetics; however, gender plays a very large part in the development of autoimmune disease. (3)
Interestingly enough, the female population accounts for about 75% of Americans afflicted by autoimmune conditions. (4) On top of that, autoimmune disease constitutes some of the leading causes of death and disability in women, up to the age of 65.
Though the relationship between sex and the prevalence of autoimmune disease is not well understood, researchers have been able to document that women have higher levels of antibodies, mounting larger inflammatory responses than men when their immune systems are triggered.
As hormones fluctuate, autoimmune diseases responds in accordance to such shifts. (5) When a women becomes pregnant, has her menstrual cycle, goes through menopause, or takes birth control, the severity of the condition may change. (6) Despite the large percentage of the female population at risk of developing an autoimmune disorder, autoimmunity is not often discussed as a potential health issue.
Commonly Diagnosed Diseases
Thyroid disease, lupus, multiple sclerosis, and rheumatoid arthritis top the list as some of the most commonly diagnoses autoimmune diseases in the United States. Let’s take a closer look at these commonly diagnosed conditions so you have a better understanding of how autoimmune disorders can impact your health.
Thyroid Disease: Graves’ disease and Hashimoto’s disease are the two types of autoimmune diseases that target the thyroid. Graves’ disease leads to an overactive thyroid (hyperthyroidism), whereas Hashimoto’s disease causes an underactive thyroid (hypothyroidism). Most individuals are diagnosed with thyroid disease between the age of 20 and 30 years old, and women have higher rates of thyroid disease compared to men.
The thyroid gland is the main metabolic regulator of the body, thus any sort of gland dysfunction affects your metabolism. In the presence of Graves’ disease, as the thyroid gland is attacked by the body’s antibodies, inflammation and swelling result. This in turn leads to hyperthyroidism, or an overactive metabolic state, whereby the body basically goes into overdrive. As the metabolic rate increases, one may also experience an increase in heart rate and blood pressure.
Hashimoto’s thyroiditis is caused by antibodies reacting against proteins on the thyroid; however, this disease is characterized by a gradual destruction of the gland itself. As the gland is destroyed, the body is no longer able to produce critical thyroid hormones required by the body, and metabolic rate will decrease, most often leading to unintentional weight gain.
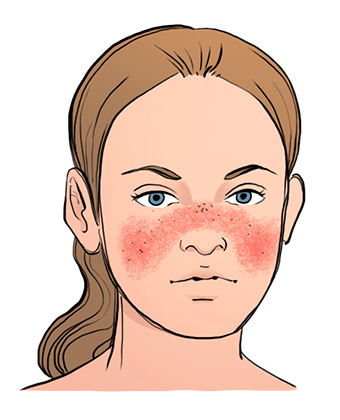
Systemic Lupus Erythematosus (SLE): SLE (i.e. “lupus), is a chronic, autoimmune disorder that affects many organs and tissues, most often skin, blood, joints, kidneys, lungs, and the heart. Antibodies produced in response to the disorder lead to the formation of immune cell complexes, which build up over time various tissues leading to pain, inflammation, or destruction of the areas of the body that are under attack.
Studies have shown that some lupus patients have low levels of DHEA (i.e. dehydroepiandrosterone), and further studies are continuing to investigate the contribution of this hormone to the onset of the disease.
Multiples Sclerosis (MS): Multiple sclerosis is a chronic inflammatory autoimmune disease, that specifically targets the central nervous system, thus impacting normal function of the brain and spinal cord.
In MS, the body produces excess antibodies that go on to specifically attack the myelin, which is a protective sheath that covers nerves. As a result of the attack, neurological, cognitive, and psychological problems set in. One may experience weakness or paralysis of limbs, numbness, vision problems, speech difficulties, problems with walking or changes to motor skills, and sexual dysfunction.
MS is actually the most commonly diagnosed neurological disease in young adults and, most often detected in between the age 20 and 40. MS, like many other conditions, is much more prevalent (almost twice as much) in women compared to men.

RA results after the body launches an autoimmune attack on the synovial membranes, the tissue that lines and cushions your joints. In response to the attack, one may experience inflammation and pain. As the condition continues to progress, the pain and swelling increase, and over time this may result in destruction and deformity of the bones.
RA typically surfaces between the age of 25 and 50, though the symptoms may be mistaken as a normal part of aging. The condition afflicts females two to four times more than males. Unfortunately, RA is rather progressive, despite treatment protcols. Many times the objective of treatment is quite simply to control inflammation, prevent or slow joint damage, hopefully leading the condition into remission.
Traditional Autoimmune Treatments
To date, there is no cure for the majority of diagnosed autoimmune disorders, thus individuals are faced with a lifetime of debilitating symptoms, which may include loss of organ or tissue function, and extensive medical costs.
The goal of treatment is most often targeted at the reduction chronic symptoms, decreasing the intensity of the immune system activity, and being able to maintain the immune system’s “normal” ability to fight foreign invaders.
Treatments vary widely and depend on the specific disease and the symptoms.
Take for example an individual living with Type I Diabetes, where the target is to replenish insulin levels, usually through injections or supplement the body with a hormone or vitamin that the body is lacking. This is much different than the treatment of an autoimmune disorder that either directly or indirectly affects the blood or the circulatory system (i.e. autoimmune hemolytic anemia, lupus, or antiphospholipidal antibody syndrome.) Treatment of these conditions may require blood transfusions.
In the case of an autoimmune disorder that affects the bones, joints, or muscle (i.e. multiple sclerosis or rheumatoid arthritis), treatment may be geared towards the maintenance of mobility or the incorporation of a medication to suppress pain and reduce inflammation.
It is also not uncommon for medicine to be prescribed as way to control or reduce the immune system’s response. Popular medications include corticosteroids and immunosuppressant drugs (i.e. azathioprine, chlorambucil, cyclophosphamide, cyclosporine, mycophenolate, and methotrexate).
Keeping Your Immune System Healthy
Keeping the immune system healthy and functioning appropriately involves taking care of your health on many different levels. Most books on the topics, as well as many health experts, promote the simple concept of “living well”.
Whole body wellness involves basic, common sense practices like following a healthy diet, getting enough rest or sleep, exercising consistently, drinking alcohol only in moderation, and avoiding stress.
To take your wellness to the next level, there are some additional steps you can take to keep your immune system healthy such as:
- Avoiding all possible exposure to environmental toxins such as mercury, poisons and heavy metals.
- Avoidance of taking unnecessary drugs.
- Choosing your foods wisely with an understanding that your diet plays a large part in healthy functioning immune system.
- Regular sexual activity has been found to be beneficial through its contribution to a healthy hormone balance.
Dietary Intervention
Now that you have a better understanding of autoimmune disease and how it can impact your health, you may be asking yourself, “Do I need to follow a Paleo gluten-free diet to help boost my immune system? What about alternative supplements or more holistic treatments?”
If you are asking yourself these questions, join the club! Of the estimated 23 million people in the United States suffering from autoimmune disease, most are asking themselves these same questions daily, hoping for a safe solution without medical and drug-related intervention.
If you suffer from an autoimmune condition, or you know of a loved one or friend who may be struggling with the condition, you may already be aware of the Autoimmune Paleo diet (AIP). Many individuals are transitioning to a refined paleo eating plan in an effort to improve life-disrupting symptoms including pain and fatigue.
While medical experts have offered mixed feedback as to how effective the Paleo diet is in treating autoimmune disease, individuals who have a vested interest in following the dietary plan consistently support the AIP, claiming that it has improved their quality of life.
While the AIP may be initiated as a way to manage an autoimmune issue, chances are those suffering from autoimmune disease also have a poorly functioning digestive tract. If the gut is not in good shape, byproducts of all of the things passing through the intestines are leaking through the gut barrier and into the blood stream, stimulating the immune system to respond with greater intensity.
The AIP is designed to help decrease inflammation and immune system stimulation at the same time.
The Standard Paleo Diet Versus The Autoimmune Paleo Diet
Many standard versions of the Paleo diet suggest starting with a strict elimination phase, meaning that the following foods should be completely avoided:
- grains
- legumes
- dairy
- refined sugars
- modern vegetable oils
- dairy, and
- processed food chemicals, including gluten.
“The Autoimmune Protocol (AIP) diet works to reduce inflammation in the intestines. Many elimination diets are not complete enough and often do not remove immune triggers that promote inflammation in the gut. AIP works to calm inflammation in the gut and also calm inflammation in the body. And while autoimmune disease can never be cured, it can be put into remission.”
When following the AIP, the basic Paleo dietary recommendations do not change; however, the protocol and dietary strategy is a more strict version. As part of the autoimmune protocol, most advocates and Paleo experts would recommend that you also avoid:
- eggs (especially egg whites)
- nuts
- seeds (including cocoa, coffee, and seed-based spices)
- nightshades (including potatoes, eggplant, sweet and hot peppers)
- alcohol
- artificial sweeteners
If you want to read more about nightshades and why they may be best to avoid as part of the AIP, here is a great resource!
While the AIP is a bit more rigid than the standard Paleo diet, it is definitely a more natural, holistic alternative to the traditional medications and treatments that over time can feel more invasive or cause a whole host of undesirable side effects.
For more information on the AIP, including a list of great tasting recipes to incorporate, check out this link!
Supplements with Promising Potential
While you should try to get in the bulk of your vitamins and minerals through your diet, there are some supplements with promising potential in reducing one’s risk of the development of autoimmune disease or as an adjunct to your treatment plan. If you are already being treated for an autoimmune condition, be sure to check with your medical provider before adding in any supplements to your diet.
Here are three supplements that are gaining attention and traction with respect to their autoimmune benefits:
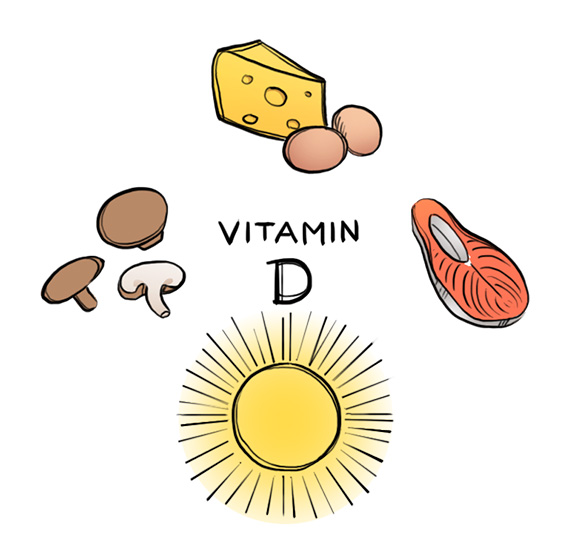
Vitamin D: One of the most intriguing areas of nutritional research involves vitamin D. For decades, science has been able to correlate a positive relationship between sunlight exposure, vitamin D levels, and autoimmune disease risk.
For example, there have been studies conducted specifically related to multiple sclerosis indicating that those living with the disease have lower levels of vitamin D than comparison groups. Interestingly enough, many autoimmune diseases, namely multiple sclerosis, type I diabetes, and lupus become more common the further away one lives from the equator.
One particular study, following subjects for 30 years, revealed that children born in Finland in 1966 who received supplemental vitamin D during the first year of life had a significantly lower risk for developing type 1 diabetes. On the other hand, children with vitamin D deficiency during the first year of life had a significantly higher risk for developing type 1 diabetes. (7)
Another study investigating vitamin D’s impact on rheumatoid arthritis, known as the The Iowa Women’s Health Study, correlated a reduced risk of RA development as vitamin D intake increased. (8) Yet another study, known as The Nurse’s Health Study, found a positive, protective relationship between vitamin D supplements and multiple sclerosis risk. (9)
Finally, a more recent study analyzing data from participants enrolled in the Multiple Sclerosis Surveillance Registry suggests that exposure to vitamin D before multiple sclerosis onset may help to slow disease-related neurodegeneration, thus causing a delay in MS progression to disability.
Why is vitamin D work so potentially beneficial to your immune system? In the 1970s, scientists discovered vitamin D receptors in many of the body’s cells (i.e. islet cells of the pancreas, lymphocytes, and colon enterocytes). Upon the discovery of the cells, further information was gathered revealing vitamin D’s ability to help keep the immune system functioning properly through the inhibition of the proliferation of T cells and further reduction in the production of proinflammatory cytokines.
Although there seems to be suggestive evidence of the benefits of vitamin D on the development of autoimmune disease, there is still much to learn. Clinical studies have not thoroughly investigated the benefit to giving large doses of vitamin D in those at risk or battling autoimmune disease. In addition, the level of vitamin D required to prevent disease and maintain health may not be the same for every individual.
Prebiotics and Probiotics: Researchers with a particular interest in autoimmune disorders have begun to question the impact of balancing the gut microbiota on the development of autoimmune disease. It appears that disruption of the intestinal ecosystem equilibrium can be traced to many disease states, including autoimmune disorders.
Prebiotics and probiotics may be a beneficial and safe therapeutic intervention for those dealing with autoimmune disease, as studies conducted within animals and humans have positively correlated the presence of probiotic cultures to enhanced activity of immunoreactive cells, thus regulating anti-inflammatory responses.
For this very reason, researchers are exploring how the gut microbiome may be different in children with type 1 diabetes versus children without the disease. (10) Other studies are linking an improvement in pain levels and self-assessed disability in adults living with rheumatoid arthritis.(11) On top of that, preliminary studies have suggested that probiotics may be of benefit for those living with colitis and inflammatory bowel disease because they may balance the gut microflora leading to a stronger intestinal defense system.
Just as stated in relation to the topic of vitamin D, the correlation between probiotics and autoimmunity is still in its preliminary phases. If this is an area of interest to you, look for future studies conducted in this area to help answer some of the unknown answers to some important questions.
Omega-3 Fatty-acids: It appears that omega-3 fatty acids can lead to promising benefits and improvements in the risk factors and treatment of autoimmune disease, particularly with those found in fish oil (i.e. EPA and DHA). According to a 2002 review of fish oil benefits, omega-3 fatty acids posses potent immunomodulatory components, which might make them rather useful in the management of autoimmune diseases.
Omega-3 fatty acids have been studied in the following autoimmune conditions:
- Arthritis
- Crohn’s disease
- Lupus
- Multiple sclerosis, and
- Rheumatoid arthritis
Researchers conducting studies out of Australia following subjects suffering from rheumatoid arthritis generated data supporting a reduction in joint tenderness and decreased use of nonsteroidal anti-inflammatory drugs with fish oil supplementation. (12) Additional studies have shown that subjects experience improvements in time to fatigue and grip strength with an increase in fish oil consumption. (13) For those suffering from systemic lupus, placebo-controlled trials indicated that omega-3 fish oils improved symptomatic disease activity. (14)
Look for further research on how omega-3 fatty acids may help to treat autoimmune disorders, and if you are interested in incorporating a fish oil supplement for other reasons, check with your medical provider before adding supplementation into your diet.
Bottom Line
When your body’s immune system is functioning just as it should, it is able to sustain a marvelous defense system, protecting your body against foreign invaders and inflammation through complex communication systems involving your cells, tissues and organs. A healthy immune system involves clear communication within the body, where it is able to tell the difference between a foreigner and itself; however, when the immune response is not functioning properly causing the communication system to breakdown, the immune response is flawed.
Autoimmune disorders develop and progress as your body’s immune system begins to attack and destroy healthy body tissue by mistake. Over time the body cannot properly regulate the intensity of the immune response causing symptoms to surface, some of which can be debilitating and painful. Symptoms associated with autoimmune disease are wide and varied, but may impact multiple biochemical processes causing dysfunction with your circulatory system, digestive system, endocrine system, urinary system, lymphatic system, respiratory system, nervous system and reproductive system.
Traditional treatment is targeted at the reduction chronic symptoms, decreasing the intensity of the immune system activity, and being able to maintain the immune system’s “normal” ability to fight foreign invaders. Non-traditional treatments that are gaining greater popularity involve lifestyle and dietary modifications, and in the future may incorporate particular supplementation protocols involving the use of vitamin D, prebiotics or probiotics, and omega-3 fatty acids.
As for dietary intervention, though there is some debate around the Autoimmune Paleo Protocol (i.e. AIP), it may be a safe and helpful dietary strategy for those who have tried just about every other treatment plan. If you need a bit more incentive to follow the AIP protocol given how rigid it may be, perhaps reading the following following resource will be a helpful motivator!
Autoimmune Disease 101 (Everything You Need to Know)
Stacey (RD, CHFS, Certified Integrative Health Coach)










No comments:
Post a Comment